Encounter Telehealth has conducted an analysis of 40 partner skilled nursing facilities in Iowa, and we are proud to announce a 6.7% drop in anti-psychotic drug use among skilled nursing facility patients between 2015 and 2018 in Iowa, alone. The analysis shows the percentage of anti-psychotic drug use among facilities in 2015, prior to working with Encounter, and in 2018 after an average of 14 months of partnering with Encounter on psychiatric care.
ABOUT ANTI-PSYCHOTICS
The Centers for Medicare and Medicaid (CMS) estimate that only a small fraction of long-term residents will ever have a condition warranting the use of anti-psychotics. However, these medications are repeatedly over-prescribed. Treating elderly patients who suffer from dementia-related psychosis with anti-psychotics puts them at a largely increased risk of death. Moreover, anti-psychotics do not improve functionality, care needs, or quality of life. Despite anti-psychotic black box warnings, these highly potent drugs are still being used to treat dementia and Alzheimer’s unnecessarily.
OVERUSE OF ANTI-PSYCHOTICS
Without access to regular, specialized psychiatric care, residents may be administered anti-psychotics off-label to treat their symptoms. Nurses and caretakers that work in these facilities are constantly exposed to physical and emotional exhaustion. This repeated exposure to stress can lead to staff burn-out. Because of this, turnover rates in long-term care are over 55% for nurses, and up to 100% for CNAs, annually. There is an ever-growing gap between supply and demand for Skilled Nurses, and the stress that comes with under-staffing is notable. In an industry already strained, anti-psychotics have been used for decades as a first resort in aggressive and physically violent patients and patients in cognitive decline.
PENALTIES AND INCENTIVES
In 2011, CMS reported that 83% of atypical anti-psychotic drug claims were for elderly nursing home residents diagnosed with conditions for which the drugs’ use was not approved by FDA. In addition, 88% of those drug claims were for residents with dementia. As a result of this report, in October of 2012, CMS partnered with federal and state agencies, nursing homes, other providers, advocacy groups, and caregivers to improve comprehensive dementia care. This partnership is known as “The National Partnership to Improve Dementia Care in Nursing Homes“. Facilities were notified that there would be a penalization for lack of reduction in anti-psychotic medication distribution. The maximum penalty is a 2% Medicare reduction. Conversely, facilities that prove a reduction in their use of anti-psychotics are eligible for an incentive. The incentive adds a maximum bonus of 1.6% to Medicare payouts.
Since 2011, CMS has reported a massive reduction of 38.9% in long-term residents using anti-psychotics. However, despite the success of the The National Partnership, a report from CMS conducted in January 2019 states “As of January 2019, there are 235 late adopter nursing homes that have been cited for noncompliance with federal regulations related to unnecessary medications or psychotropic medications two or more times since January 1, 2016, and who have not shown improvement in their long-stay anti-psychotic medication rates.”
ENCOUNTER‘S PART IN REDUCING ANTI-PSYCHOTICS
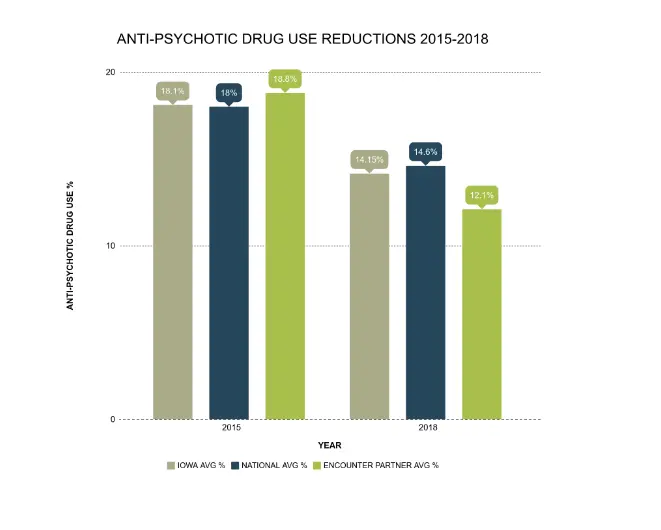
Of the 443 nursing homes in Iowa, the 40 facilities that Encounter Telehealth partners with have shown an average 6.7% reduction in the use of anti-psychotics from 2015 to 2018.
Some of Encounter’s facilities have shown notably large reductions. One facility went from 28.6% of residents using anti-psychotics in 2015 to a low 7.3% in 2018. That is a 21.3% decrease in the usage of anti-psychotics, and nearly one half of the current national average. Facilities in Iowa that partnered with Encounter Telehealth had an average 12.1% of residents on anti-psychotic medications as of 2018. That is 2.4% below the average of total Iowa nursing homes.
Through Encounter Telehealth, patients receive evaluations and psychiatric medication management services from Psychiatric Mental Health Nurse Practitioners. This ensures proper diagnoses and medication management from the convenience of the facility. Encounter also offers talk therapy, which has been proven to be beneficial to patients with dementia and cognitive decline. In fact, many studies indicate that patients do better when medication and talk therapy are used together, than when either of them is used alone. In addition, Encounter provides staff training. Proper staff training can ensure quality healthcare and safety for everyone. In training staff to use alternative, non-pharmacological interventions, studies have shown statistical benefits in patients with dementia.
In addition, Encounter Telehealth helps to reduce staff stress by providing quality healthcare within the convenience of the facility. Nurses are no longer required to organize transportation and be removed from the facility to get patients to appointments. Provided that the facility has an internet connection, Encounter can see patients without any disruption. This is extremely beneficial for patients with dementia and other cognitive impairments.
WRAPPING UP
At Encounter Telehealth, we are committed to providing compassionate, consistent, and quality care. Our providers include Clinical Nurse Specialists (CNS), Licensed Clinical Social Workers (LCSW), and Psychiatric Mental Health Nurse Practitioners (PMHNP). Our services include evaluations, psychiatric medication management, behavioral healthcare, therapy, and staff training. Encounter Telehealth also works with local primary care providers, facility staff and other caregivers to ensure a holistic approach to the patient’s needs. We are proud of the evident reduction in the use of anti-psychotics among our partner facilities. We strive to continue providing quality care and results. Please view our report, Encounter Telehealth Anti-Psychotic Reduction, HERE.